Dry Eye Management
Dysfunctional tear syndrome can be caused by multiple factors, and can evolve due to insufficient tear production, poor tear quality, or poor tear distribution over the ocular surface. Dr. Milner has specialized in DTS management his entire career and has recently published his approach as a wide sweeping treatment algorithm including both on and off-label therapies for management. He has been invited to speak about his treatments throughout the United States and abroad.
Who doesn’t love fresh blooms, breezy weather, sunny skies—and burning eyes, if you have a condition known as dry eye, which can be exacerbated by the itching and tearing brought on by seasonal allergies.A 24-Hour Guide to Improving Your Allergy Symptoms
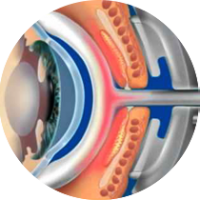
What many longtime dry eye sufferers may not realize is that it’s often caused by Meibomian gland dysfunction (MGD), which occurs when the tiny Meibomian glands in eyelids become stopped up and unable to protect the tear film—a thin layer of fluid that covers the outer surface of the eye.
While MGD has traditionally been hard to treat, there’s a breakthrough therapy that’s making it far simpler to do: the LipiFlow® Thermal Pulsation System, which uses a cutting-edge device to heat up and massage away the blockage in just 12 minutes, right in your eye doctor’s office.
Although you may never have heard of this disorder, it’s actually quite common: More than 20 million Americans have dry eye. And according to one 2012 study published in the journal Cornea, 86% of study participants with dry eye also had symptoms of MGD.
The most likely culprit is poor blinking. The science of blinking is downright fascinating: Every time we do so, we activate the muscles around our Meibomian glands, squeezing each one and causing the functional glands to secrete a droplet into the tear film. Those droplets fall into your tear film and create its lipid layer, or the outermost layer, When you’re not blinking fully or frequently enough, the lipid layer stays stagnant, turning from a nice olive oil consistency to more of a thicker oil. This blocks the gland, leading to the symptoms we classically associate with dry eye, such as burning and itching. Anyone can get MGD, but some of us are more prone than others. Contact lens wearers are at higher risk, as are heavy users of electronic devices. Postmenopausal women are also at higher risk for MGD.
Eventually, if a Meibomian gland stays plugged up with that thick white stuff for long enough, it will die off, and your symptoms will grow even worse. (Your tear film has two other layers, composed of water and mucus. Cases of dry eye that aren’t caused by MGD may be caused by problems with these other layers, and result in the same burning, itchy sensation.)5 Things Your Contact Lenses Wish They Could Tell You
Anyone can get MGD, but some of us are more prone to it than others. Contact lens wearers are at higher risk, for instance, as are heavy users of personal electronic devices. Both have a much lower blink rate. If you’re working on a computer, your blink rate drops in half.
Postmenopausal women are also at higher risk for MGD, as well as people with autoimmune disorders, like rheumatoid arthritis and lupus. Taking certain medications, including beta-blockers and antihistamines, can also increase your odds of having MGD. Even the weather can exacerbate the condition—dry and windy conditions are particularly apt to trigger the ocular misery.
Historically, ophthalmologists and optometrists have had to try and clear blockages in the Meibomian glands by physically squeezing the eyelid—a sometimes painful and not-always-effective remedy. Today, we have multiple devices to help treat this disease.
Lipiflow
Research published in the journal Clinical Ophthalmology supports its effectiveness: The study showed that treatment with the device increased the average amount of time that contact lens wearers with MGD could comfortably wear their lenses by approximately four hours.
Curious to learn more about how it works? The procedure is done in just four simple steps:

1. First, your eye doctor will use the LipiScan imagingdevice to examine your Meibomian glands. This will help your doctor make a diagnosis, which may involve additional testing.
2. If it’s determined that you do have MGD, you can proceed with receiving the 12-minute LipiFlowtreatment.Before it begins, your doctor will use numbing drops (the same ones routinely used at yearly eye exams) to help ease any potential discomfort from the procedure.
3. Next, the system’s activators—dome-shaped, single-use sterile devices—are placed on your eyes. Their vaulted shape keeps your corneas protected during the treatment, which focuses on the inner eyelids, where the Meibomian glands are located.
4. Using what’s called Vector Thermal Pulsation technology, the activators send heat into the glands inside your lids. This combination of heat plus pressure massages any blockages and liquefies and clears the obstructions that are causing your symptoms.
Learn more about the LipiFlow® Thermal Pulsation System, including safety information.
ILux
ILux is another option for patients that suffer from MGD. The procedure is similar to lipiflow but is better suited to patients with certain anatomic variations.

Blephex
Blephex is a device to treat anterior manifestations of blepharitis. The motorized tip is designed to remove all debris from the eyelashes as well as any biofilm that has formed on the lids and is blocking the meibomian glands.

